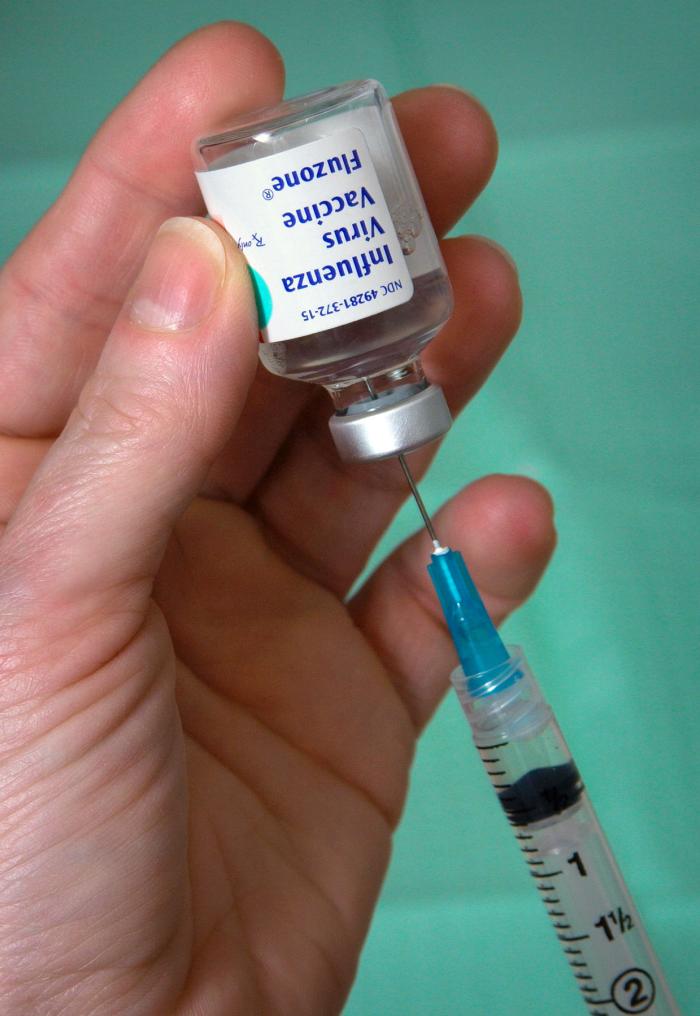
 Immunity is the ability of our bodies to resist almost all types of organisms or toxins that tend to damage our tissues and organs. Much of immunity is acquired immunity, which means it does not develop until after the body is first attacked by an invader. Acquired immunity is caused by a specific immune response in our bodies, and can provide us with extreme protection against toxins. For this reason, immunization plays a vital role in keeping us healthy. We are immunized when injected with a vaccine, or an organism that has lost its pathogenic abilities. Today, vaccines can be manufactured for whooping cough, diphtheria, tetanus, measles, smallpox, and many other diseases.
Immunity is the ability of our bodies to resist almost all types of organisms or toxins that tend to damage our tissues and organs. Much of immunity is acquired immunity, which means it does not develop until after the body is first attacked by an invader. Acquired immunity is caused by a specific immune response in our bodies, and can provide us with extreme protection against toxins. For this reason, immunization plays a vital role in keeping us healthy. We are immunized when injected with a vaccine, or an organism that has lost its pathogenic abilities. Today, vaccines can be manufactured for whooping cough, diphtheria, tetanus, measles, smallpox, and many other diseases.
Pathogens Wear Uniforms
Since our bodies must first be introduced to a pathogen in order to initiate the acquired immune response, we must also have a mechanism for recognizing the invasion. Every cell in the body has a unique set of molecules that cover their surface, almost acting as a uniform. Pathogens, however, can also wear a unique uniform of marker molecules, called antigens, as shown in the figure below:
Antigens are commonly proteins or large polysaccharides that are not naturally on the cells of a person’s body. Antigens play a crucial role in the function of vaccines. They help our immune system distinguish between cells that are part of our body, and invading pathogens that need to be destroyed.

Swine Strain of Influenza Virus
The image on the right is a model of a swine strain of influenza virus. The blue structures are antigens called hemagglutinin glycoproteins. There are sixteen types of hemagglutinin glycoproteins that are found on influenza viruses, and each type can undergo slight changes due to mutated genes. These slight changes in the antigen are why we constantly produce new flu vaccines to administer every year–we must train our bodies to recognize the new invaders!
Vaccines help us do this training by exposing our bodies to the pathogen’s antigens, and initiating an immune response. It is important to understand that the entire pathogen is not needed to instigate a response. Many vaccines, such as the meningococcal vaccine, do not contain the entire pathogen, but rather separated antigens from the pathogen. Similarly, vaccines can also employ antigens on a dead pathogen and antigens on a live-weakened pathogen.
Vaccines Initiate a Response

Phagocytosis of a pathogen.
Once vaccines have exposed our bodies to a pathogen, our macrophage cells begin ingesting the pathogens via phagocytosis. The image on the left depicts phagocytosis, during which a macrophage will engulf a pathogen and release the pathogen’s antigens into its own cell body.
Macrophages take these engulfed antigens and pass them by cell-to-cell contact directly to adjacent lymphocytes, like B cells and T cells.

Streptococcus pneumoniae with polysaccharide antigens and carrier protein.
The effectiveness of an antigen to activate B and T cells depends on its epitopes, or recurring molecular groups, as shown in the earlier figure of a pathogen’s marker molecules. If the antigen is made of protein, both B cell and T cell reactions will be initiated. If the antigens is made of polysaccharide, only B cell reactions are induced. This concept must be taken into account when manufacturing vaccines. For instance, as shown in the image on the right, polysaccharide antigens are sometimes coupled with carrier proteins in the vaccine, such that the vaccine will induce both T cell and B cell reactions for better immunity.
Our Body’s Soldiers
B cell and T cell lymphocytes fight against foreign invaders in different, but equally important ways.
T cells assist in the immune response both directly and indirectly. Cytotoxic T cells fight against foreign invaders in a direct way, by recognizing and killing infected or damaged cells. Helper T cells, on the other hand, work indirectly by releasing cytokines, or chemical instructions, to the rest of the immune system. This allows for a more specialized immune response that will ultimately be more successful.

Antibodies bind to the epitope of an antigen.
The primary role of B cells is to produce antibodies, also called immunoglobulin molecules. The antibodies produced by the B cells are unique to the antigen of the invader, resulting in a highly specific immune response. It is these antibodies that will enable the long-term immunity provided by vaccines, but first we must understand what role they play.

Immunoglobulin A, a crucial antibody.
Take for instance Immunoglobulin A, shown right, the most abundant antibody in the human body. This antibody class serves to fight against specific micro-organisms in the mucosal linings of the body, and is unable to fight against any other invaders. This is due to the specificity of antibodies, as they only bind to one antigen. While antibodies provide a powerful method of fighting against diseases, their specificity and the amount of time it takes to produce them allows foreign invaders to inflict damage before being halted. However, the immune system has a way to prevent previously encountered pathogens from successfully attacking again. This is accomplished by retaining an immune memory, thereby allowing for the quick production and release of the antibody specific to the returning invader.
Immune Memory
When the T cells are destroying the pathogen faster than it is reproducing, the immune system wins and the virus disappears. After fighting off an infection, the body retains some of its B and T cells as memory cells. Memory cells are also specific to the antigen that the body just eliminated, so if the body ever comes into contact with it again, the immune system can initiate a response quickly.
This concept of memory cells is the reason why vaccines provide our bodies with extended protection against pathogens. Since vaccines employ a dead or weakened form of the pathogen, the body is tricked into preparing for battle. Thus, B and T cells are created for the pathogen, and then retained for future use. Your immune system is now ready to defend your body if you are ever exposed to the pathogen again.
References
Image One: http://upload.wikimedia.org/wikipedia/commons/f/f6/Fluzone_vaccine_extracting.jpg
Image Two: modified from http://classconnection.s3.amazonaws.com/301/flashcards/2756301/jpg/picture11360549935810.jpg
Image Three: http://upload.wikimedia.org/wikipedia/commons/0/02/Flu_und_legende_color_c.jpg
Image Four: http://www.flickr.com/photos/zeissmicro/8765512496/
Image Five: http://upload.wikimedia.org/wikipedia/commons/thumb/2/20/Streptococcus_pneumoniae.jpg/240px-Streptococcus_pneumoniae.jpg
Image Six: http://askabiologist.asu.edu/b-cell
Image Seven: http://dict.space.4goo.net/dict?q=antibody
Image Eight: http://upload.wikimedia.org/wikipedia/commons/d/dd/Ig_A.jpg
http://www.ncbi.nlm.nih.gov/pubmed/7505396
http://www.ncbi.nlm.nih.gov/books/NBK10770/
http://www.sinobiological.com/Influenza-Hemagglutinin-Subtypes-and-Flu-Virus-Strains-a-144.html
Guyton, A.C. et al. 2000. Textbook of Medical Physiology. 10th ed. Saunders.
Sadava, D. et al. 2011. Life: The Science of Biology. 11th ed. Sinauer Associates, Inc. and W.H. Freeman and Company.



You actually make it seem really easy together with your
presentation but I to find this matter to be really something which I feel I would never understand.
It sort of feels too complex and very extensive for me. I am taking a look forward in your next submit, I’ll attempt to
get the hold of it!
Hello, I thought this was a great article. Thank you for sharing.